Abstract
Background: Varicella zoster virus (VZV) infection is a common complication after hematopoietic stem cell transplantation (HCT) and occurs in 16%-41% of transplant recipients, with a relatively high incidence. Although localized dermatomal rashes are a typical symptom of VZV infection, dissemination to internal organs and secondary bacterial infections are occasionally fatal. Furthermore, patient quality of life is impaired by postherpetic neuralgia. To reduce the incidence of VZV infection after HCT, the efficacy of long-term acyclovir prophylaxis has been evaluated. Several studies concluded that VZV infection was suppressed during prophylaxis, but increased after acyclovir discontinuation, i.e., rebound effect exists. We conducted a meta-analysis to evaluate the efficacy of acyclovir prophylaxis against VZV infection after HCT and whether rebound effect really exists or not.
Methods: Medline, Embase plus Embase classics, and Cochrane Central Register of Controlled Trials were used for systematic review of studies from 1980 to June 23, 2017, without language restrictions. The literature search strategies used Medical Subject Headings and free text words related to "acyclovir," "hematopoietic stem cell transplantation," and "varicella zoster virus." Exclusion criteria were animal or in vitro studies, case control studies, and case reports. Intervention of this research was defined as acyclovir prophylaxis after HCT.
We used the Cochrane Collaboration's Risk of Bias tool and Newcastle-Ottawa Quality Assessment Scale (NOS ) to evaluate the study quality. The primary outcome was to evaluate the incidence of VZV infection within the first year after acyclovir discontinuation compared with that in patients without acyclovir prophylaxis. The secondary outcome was the risk of VZV infection/reactivation during acyclovir prophylaxis after HCT. Subgroup analyses were conducted according to acyclovir dose (>400 or ≤400 mg), duration of acyclovir treatment (>6 or ≤6 months), and presence of disseminated disease. We conducted a sensitivity analysis for studies with a NOS score of ≥7 points. The analysis was conducted using Review Manager Version 5.3. We performed a meta-analysis using fixed effect models with risk ratio (RR) and a 95% confidence interval (CI). Heterogeneity was assessed using the chi-squared test and I-squared statistic. Publication bias was assessed with funnel plots.
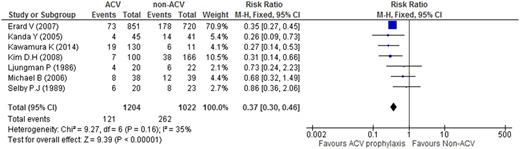
Results: Of 1,803 studies from the search database, seven studies with a total of 2,226 patients were eligible. Patients were divided into the acyclovir prophylaxis (n = 1,204) and no prophylaxis groups (n = 1,022). We compared the incidence of VZV infection between the two groups, within 1 year after discontinuing acyclovir prophylaxis in the acyclovir prophylaxis group and without any acyclovir after HCT in the no prophylaxis group . Results showed that acyclovir prophylaxis significantly reduced the incidence of VZV infection (RR: 0.37, 95% CI: 0.30-0.46, heterogeneity I2 = 35%, χ2 = 9.27). The risk of VZV infection/reactivation during acyclovir prophylaxis was reduced (RR: 0.17, 95% CI: 0.12-0.24, heterogeneity I2 = 0%, χ2 = 0.41). Among four studies that reported disseminated disease, acyclovir prophylaxis reduced the RR of disseminated disease (RR: 0.31, 95% CI: 0.19-0.58, heterogeneity I2 = 0%, χ2 = 1.02). The analysis of four studies reporting acyclovir prophylaxis for >6 months indicated that longer prophylaxis reduced the RR of VZV infection (RR: 0.34, 95% CI: 0.27-0.43, heterogeneity I2 = 48%, χ2 = 5.80). Patients receiving low-dose acyclovir showed significant reduction in the incidence of VZV infection (RR: 0.31, high 95% CI: 0.18-0.54). Results of the sensitivity analysis for studies with NOS score of ≥7 points showed significant reduction in the incidence of VZV infection with acyclovir prophylaxis (RR: 0.43, 95% CI: 0.30-0.62, heterogeneity I2 = 39%, χ2 = 8.24).
Conclusions: This study showed that long-term acyclovir prophylaxis significantly reduced the incidence of VZV infection even after its discontinuation compared with no treatment and indicated that rebound effect did not exist. Long-term acyclovir prophylaxis for VZV infection after HCT is effective during and after therapy. This study also showed that low dose was sufficient for VZV prophylaxis. Based on our results, we recommend long-term prophylaxis for >6 months.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal